Osteoporosis and its precursor osteopenia are conditions that weaken bones, making them brittle and more prone to fractures. It’s often called the “silent disease” because it progresses without symptoms until a break occurs. As we age, maintaining strong bones becomes critical, and for those with osteoporosis or osteopenia, managing bone health requires a comprehensive approach. Understanding osteoporosis and utilizing physical therapy are key to strengthening bones, enhancing stability, and reducing the risk of falls.
In this post, we’ll dive into the science behind osteoporosis, explain how physical therapy can help, and offer tips on strengthening bones and improving stability.
Understanding Osteoporosis and Osteopenia | The Science Behind It
Our bones are constantly undergoing a process called remodeling, where old bone tissue is broken down (resorption) and new tissue is formed (formation).
Osteopenia is a condition where bone density is lower than normal but not low enough to be classified as osteoporosis. It’s often seen as a precursor to osteoporosis and indicates that bones are weaker than they should be, which increases the risk of fractures over time.
Osteoporosis occurs when this balance shifts and bone resorption happens faster than bone formation. This leads to a decrease in bone density.
For simplicity, we’ll use the term “osteoporosis” throughout this discussion, but the information provided applies to both osteoporosis and osteopenia.
Several factors contribute to the development of osteoporosis, including aging, hormonal changes (particularly in women after menopause), genetics, and lifestyle choices such as diet and physical activity. People, women more than men, with a slender frame, and small wrists, and ankles tend to get osteoporosis.
Calcium and vitamin D deficiencies also play a role, as these nutrients are critical for bone health. But honestly, most of us are deficient in many important vitamins and minerals.
Certain medications, such as prolonged use of corticosteroids, can contribute to osteoporosis by reducing bone density. Other medications, including some chemotherapy drugs, thyroid medications, and certain antiepileptics, may also lead to bone loss over time. These treatments can interfere with the body’s ability to absorb calcium and build healthy bone tissue, further increasing the risk of fractures and osteoporosis.
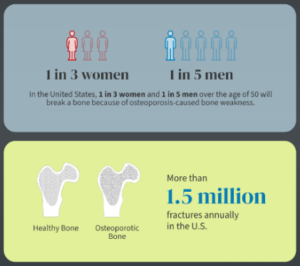
Osteoporosis affects women more than men, though many men do have osteoporosis as well.
A bone density test (DEXA scan) measures bone mineral density (BMD) determining the severity of bone loss whether it’s osteopenia or osteoporosis. A lower BMD increases the risk of fractures, especially in the spine, hips, and wrists. AMA guidelines recommend a DEXA scan for women at age 65 and men at age 70.
Physical Therapy’s Role in Strengthening Bones
Often the first person to recognize that a person may have osteoporosis is the physical therapist as there are postural changes that are typical of someone who has osteoporosis. Postural changes we might see:
- The thoracic (upper) spine will become more kyphotic (rounded/hunched) with an increased lumbar (lower spine) lordosis called a kypholordotic posture.
- Your thoracic and lumbar spine may become very flat, losing any natural curvature.
- You may even have scoliosis, your spine forms an S shape, for the first time in your life.
- The distance between the bottom of your rib cage and the top of your pelvis has decreased significantly.
These spinal changes are caused by the vertebral bodies collapsing on themselves to become shorter as well as the discs between the vertebral bodies degenerating and having less fluid which is why you are now shorter than you have been your whole life.
I find the AMA guidelines of waiting till 65 to be too late as I have seen many people with these telltale signs of postural changes at a much earlier age and ultimately are diagnosed with osteoporosis. If you have any of the risk factors or postural changes You will have to be proactive and ask your physician for a DEXA scan much earlier than age 65.
Combatting Osteoporosis
One of the best ways to combat osteoporosis is regular physical activity, especially weight-bearing and resistance exercises that stimulate bone growth. Physical therapy can help people with osteoporosis by designing personalized exercise programs to strengthen bones, improve muscle strength, and increase mobility.
- Weight-Bearing Exercises: Activities like walking, jogging, stair climbing, and resistance training help stimulate bone growth. These exercises place pressure on the bones, encouraging the body to build more bone tissue to accommodate the stress.
- Improving Muscular Strength: Strong muscles support and protect bones, reducing the likelihood of fractures. A physical therapist may introduce resistance training exercises, such as using resistance bands, weights, or bodyweight movements, to strengthen muscles and protect fragile bones.
- Posture and Alignment: Good posture is essential for distributing weight evenly across the skeleton, especially in individuals with osteoporosis. Core-strengthening exercises like planks or bridges, not situps or crunches, can improve posture and provide better support for the spine. You want to avoid abdominal crunches or situps as this puts too much pressure on your already collapsing vertebrae.
Stability and Fall Prevention
As bone density decreases, the risk of fractures from falls increases. Physical therapy also emphasizes stability and balance training to reduce this risk.
- Balance Training: Exercises that focus on balance can improve stability and proprioception (your body’s ability to sense where it is in space). Simple exercises like single-leg stands or using a balance cushion can make a big difference in preventing falls.
- Assistive Devices: In some cases, a physical therapist may recommend assistive devices such as canes or walkers to improve mobility and prevent falls. Learning to use these devices properly can help maintain independence and reduce fall risk.
- Environmental Modifications: Making small changes at home, like removing tripping hazards, adding grab bars in the bathroom, and ensuring good lighting, can significantly reduce the risk of falling and fracturing a bone.
Specialized Tools and Modalities for Bone Health
For those looking for additional ways to manage osteoporosis, tools like the bioDensity machine and the Power Plate can be highly beneficial.
- bioDensity Machine: This device allows users to perform four isometric exercises that load the bones with a controlled amount of stress. The bioDensity machine is designed to target bone growth by stimulating the musculoskeletal system with multiple times the user’s body weight. It’s safe for most individuals and can be an effective tool in reversing osteoporosis over time.
- Power Plate: The Power Plate is a vibration platform that moves in three dimensions, stimulating the body’s small stabilizing muscles. Exercises performed on the Power Plate, like squats or planks, help improve strength and balance. It’s particularly useful in preventing falls and maintaining stability.
Nutrition and Lifestyle Adjustments
No discussion about bone health is complete without addressing the importance of nutrition. Adequate intake of calcium and vitamin D is crucial for building and maintaining strong bones. Adults need around 1,000–1,200 mg of calcium per day, which can be obtained from foods like dairy products, leafy greens, and fortified foods. Vitamin D, often acquired from sunlight, helps the body absorb calcium and should be supplemented if levels are low.
Additionally, lifestyle changes can make a big difference. Avoiding smoking and limiting alcohol consumption both have positive effects on bone health. Regular physical activity, a balanced diet, and avoiding activities that increase the risk of falls are all critical steps in managing osteoporosis.
Medical management of Osteoporosis
Your doctor may prescribe bisphosphonates such as Fosamax or Reclast, denosumab (Prolia), or hormone replacement therapy (HRT), which may be necessary to slow bone loss.
A Holistic Approach to Managing Osteoporosis
Managing osteopenia and osteoporosis effectively requires a comprehensive, holistic approach that addresses the root causes and supports long-term health. This includes personalized physical therapy to strengthen bones and improve stability, a nutrient-rich diet, and consistent exercise to maintain bone density. Supplements and vitamins, particularly calcium and vitamin D, can fill nutritional gaps, while lifestyle changes further enhance bone health. In some cases, medications may also be part of the treatment plan. By collaborating with your healthcare provider and physical therapist, you can develop a tailored strategy that promotes overall well-being and helps you stay active and resilient despite osteoporosis.







Leave a Reply