I don’t remember learning about hypermobility syndromes when I was in PT school in the 80s or even having seen this diagnosis as recently as 2010. It didn’t show up on my radar until I had a patient with Ehler-Danlos Syndrome in 2011. In recent years, I have been noticing that more and more of my patients have hypermobility. I can’t explain why I am seeing this more often other than, now that I know better, I do better.
The first clue I look for when diagnosing hypermobility is in their history and a description of their symptoms and how they got them. They may have chronic pain, tend to be injury-prone since childhood, have had injuries that take a long time to heal, have complaints of tightness coupled with high flexibility, or have been to many health professionals to help them feel better with various diagnoses.
What is Hypermobility Syndrome?
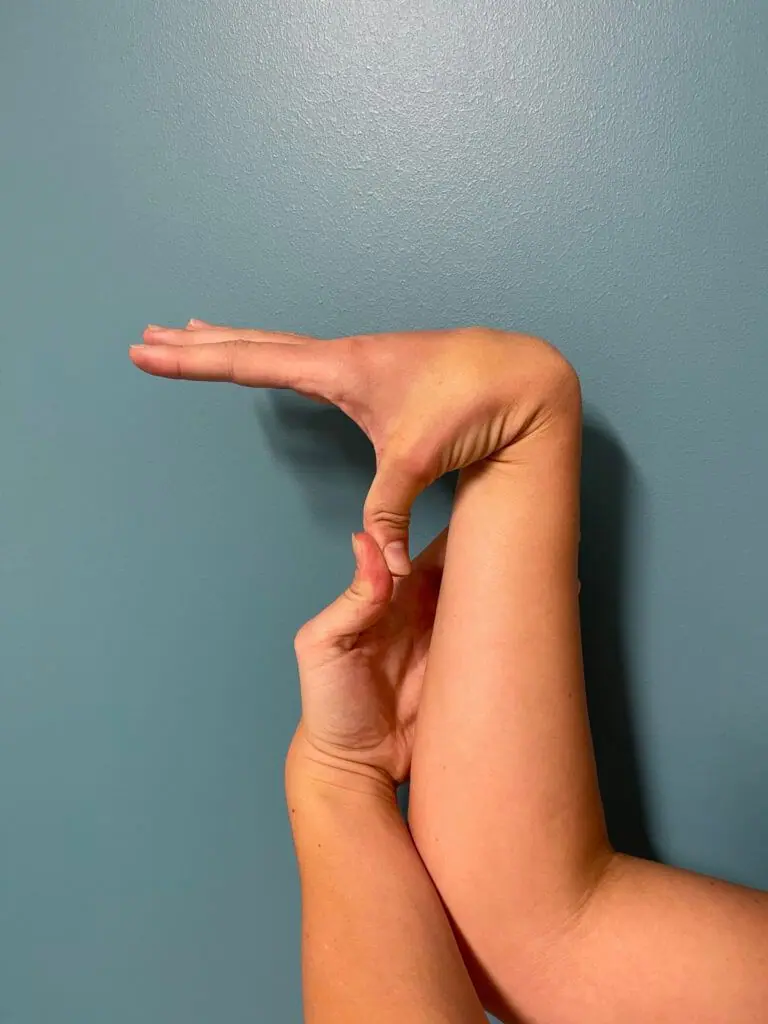 Hypermobility syndrome occurs when joints have an unusually large range of motion. This can sometimes lead to pain, muscle fatigue, or even frequent injuries. Some people with hypermobility can move their joints in ways that look a bit extreme—like bending fingers backward or extending knees beyond the usual straight line. This joint instability can lead to chronic pain and difficulty with everyday activities. To initially test to determine if you are hypermobile, try using the Beighton Scoring System.
Hypermobility syndrome occurs when joints have an unusually large range of motion. This can sometimes lead to pain, muscle fatigue, or even frequent injuries. Some people with hypermobility can move their joints in ways that look a bit extreme—like bending fingers backward or extending knees beyond the usual straight line. This joint instability can lead to chronic pain and difficulty with everyday activities. To initially test to determine if you are hypermobile, try using the Beighton Scoring System.
For those experiencing discomfort, managing it starts with knowing your body’s unique needs and working with professionals who can help you build joint strength and stability to prevent injury.
Examples of Hypermobility
By the time my client Sean came to me, he had had 5 years of constant sacroiliac (SI) pain when sitting. He had seen multiple medical professionals without relief. His SI pain began after rolling over in bed. He works out regularly but cannot do overhead lifting over 25 lbs, as his shoulders “feel like they will pop out”. He also complained of very tight hamstrings but would describe himself as flexible.
Have you ever been called “double-jointed” or noticed that you can bend certain joints in ways others can’t? Like my patient, Craig, who was told his shoulders looked like they were dislocating while swimming the butterfly, or Dana, as a teenager, could do the splits way past straight and has had hamstring pain ever since.
While it might seem like a neat trick, being extremely flexible can actually be a sign of a condition called hypermobility syndrome—or, in some cases, a more complex condition like hypermobile Ehlers-Danlos Syndrome (hEDS) or Ehlers-Danlos Syndrome (EDS). Each of these conditions comes with challenges, but understanding their differences can help you manage symptoms, find ways to reduce pain, and stay as active and healthy as possible to prevent future complications such as joint replacement surgery.
Hypermobile Ehlers-Danlos Syndrome (hEDS)
Hypermobile Ehlers-Danlos Syndrome (hEDS) is a genetic condition that goes beyond hypermobility and affects connective tissues throughout the body, not just in the joints. People with hEDS experience symptoms like digestive issues, fatigue, easily bruised skin, and slow wound healing. While many of these symptoms seem unrelated, they stem from the same underlying problem—hEDS affects collagen, an essential protein in connective tissue that provides stability and strength throughout the body.
One of the biggest challenges with hEDS is getting a proper diagnosis through genetic testing. Symptoms of hEDS overlap with other conditions such as fibromyalgia, which can make diagnosis tricky. However, recognizing these signs and seeking the right support is essential. The approach to managing hEDS often requires more comprehensive treatment to address the condition’s varied symptoms.
Ehlers-Danlos Syndrome (EDS)
Ehlers-Danlos Syndrome (EDS) is actually a group of genetic disorders affecting connective tissue in the body, not just in the joints but also in the skin, blood vessels, and even organs. There are 13 recognized subtypes of EDS, with hypermobile EDS being one of them. People with EDS may notice that their skin is fragile, that they bruise easily, or that they have difficulty maintaining joint stability. In more severe cases, EDS can even lead to complications in blood vessels or organs, highlighting the need for an individualized approach to treatment.
While there’s no cure for hypermobility or EDS, physical therapy can play a major role in managing symptoms.
Managing Hypermobility and EDS through Physical Therapy
Physical therapy can be a powerful tool for managing hypermobility and EDS. It helps individuals strengthen the muscles surrounding hypermobile joints, reducing the risk of injury and improving stability and ultimately preventing subluxations (partial joint dislocation) or full dislocations. The focus is on building core stability, joint control, and alignment, creating a foundation of strength that supports hypermobile joints without putting too much strain on them. In addition, a lot of education will be provided to learn how to best manage your flexible body with movement, exercise, everyday activities, and positioning. After 2 months of PT Sean now has intermittent and less intense SI pain, as well as improved postural alignment that also contributed to his pain.
“Previous rounds of PT left me with multiple injuries and little progress. So when a colleague of mine told me about IMT, I quickly looked into IMT and found Denise Schwartz at The Manual Touch. This past year I have made progress in physical therapy for the first time since being symptomatic with EDS, and I know that in the positive and uplifting environment in which Denise provides I can continue to make gains.
I feel very fortunate to have Denise in my life as a physical therapist who listens to me, is patient, compassionate, and who continuously strives to provide the best care possible for my condition.” – Megan B. Arlington Heights
A personalized physical therapy plan will include strength, neuromuscular control (how your body works together), proprioceptive (knowing where your body is in space), and balance exercises that can be adjusted based on each person’s needs. For people with hEDS or EDS, physical therapy emphasizes not just general strength but also the precise control needed to prevent injuries from repetitive movements or poor posture. With the right guidance, physical therapy becomes a tool to help you live with hypermobility or EDS more comfortably and confidently.
Everyday Tips for Living with Hypermobility, hEDS, or EDS
Making small adjustments, like using proper body mechanics, taking breaks during repetitive tasks, and even using supportive devices when needed, can be incredibly helpful. Finding ways to relieve strain on your joints can also prevent further discomfort. Connecting with online communities, such as The Ehlers-Danlos Society, can provide additional resources and support. Sometimes, learning from others with similar experiences can offer valuable insights and encouragement.
Living with hypermobility or EDS can make daily life a little more complicated and not easy, but with the right care and a better understanding of your condition, an active, pain-free life is within reach. Whether it’s through physical therapy, lifestyle adjustments, or connecting with a supportive community, there are effective ways to manage your symptoms.
If you’re experiencing hypermobility-related symptoms or have been diagnosed with EDS, a comprehensive physical therapy plan could be the next step in your journey toward building strength, stability, and resilience. We at The Manual Touch have great experience working with patients with hypermobility issues.







Leave a Reply